Unintended Consequences and the Huge Epidemic You Don’t Hear About
“The number of yearly U.S. MRSA deaths per citizen is more than triple the rate of U.S. polio deaths during the peak of the polio epidemic.”
Adapted excerpt from book by award-winning 3-time author:
Linda F. Palmer, DC
“Baby Poop: What Your Pediatrician May Not Tell You… about Colic, Reflux, Constipation, Green Stools, Food Allergies, and Your Child’s Immune Health”
Opportunistic Bacteria
A number of factors can lower your immune system and can create an environment for bacteria to take advantage of a situation, invade, and to flourish. A harsh cold virus and/or the use of antibiotics—possibly combined with other weakening factors such as a less-than-optimal diet, insufficient sleep, inadequate sun, or low levels of exercise—can awaken otherwise quiet bacteria in an individual’s respiratory system or gut. These bacteria are referred to as opportunistic; they can invade, overgrow, and cause, for example, a sinus infection or diarrhea when the opportunity arises.
Wipe Them All Out?
On first thought, it seems that we should just wipe out any bacteria in our collective human microbiome that could possibly cause illness, but hard lessons are being learned today from that very effort. Our human microbiome seems to have settled over the millennia into a best possible situation in which certain opportunistic bacteria are maintained so that they keep out much more serious microbes by competing for attachment sites on the intestinal walls and for nutrients. It is these lesser bullies that challenge greater bullies and that are responsible for preventing frequent and dire illnesses in all of us.
Good Efforts Gone Bad
Scientists have recognized for many decades now that the use of antibiotic drugs has a downside. Though these antibiotics have acted as miracle life savers, their overuse is causing more and more drug-resistant strains of opportunistic bacteria to develop and spread. Of great concern is the fact that some of these are showing up to be even more potent than the original strains.
Competition Removed
Unsuspected villains have also caused serious consequences. A highly unexpected misfortune has grown out of the pneumococcal vaccination program. Pneumococcal vaccines fight against potentially dangerous pneumococcal pneumonia, meningitis, and infections of the heart. It’s been discovered that a different kind of bacteria, called Staphylococcus aureus and known as staph for short, has replaced part of the niche in our microbiota created by the reduction of pneumococcal strains (also known as Streptococcus pneumoniae) via pneumococcal vaccines.
Unintended Consequences
It’s becoming evident to researchers that pneumococci and S. aureus have been competitors within human microbiomes. Pneumococcal bacteria were apparently keeping more serious staph infections at bay but now S. aureus has expanded greatly throughout populations globally. Once practically unheard of, suddenly S. aureus was causing flesh-eating bacteria to become a household term. This once-rare infection became more prevalent than anyone would wish to see. The new invading flesh-eating bacteria have been coming from a newly prevalent strain of S. aureus that has since been monikered methicillin-resistant S. aureus, or MRSA (pronounced “mersa”). The name MRSA was given because these bacteria, which can cause several types of very serious or even deadly infections including pneumonia, are resistant to common antibiotic drugs (methicillin). Over-use of antibiotic drugs (another tampering with human collective flora) is responsible for the drug resistance of this bacterium, whereas reduction of pneumococcal bacteria from the human microbiome has allowed MRSA to flourish.
A Rapidly Spreading Epidemic
Since the year 2000, the same year that the pneumococcal vaccines began,
infections that were rare and limited to hospital patients who had been treated
with antibiotics began suddenly popping up in previously healthy children and
adults throughout the community who had not been hospitalized and had not
been taking antibiotics—and the trend has continued.
In England, a study compared 2003 rates of various MRSA infections with those prior to the introduction of the pneumococcal vaccine. They found serious staph skin infections of impetigo and scalded skin syndrome increased by 5 to 8 times for children under
4, and dangerous staph blood infections increased by 2 to 6 times.
The Numbers
MRSA deaths have been reported by the CDC as 6.3 in 100,000. By comparison, U.S. deaths from HIV (AIDS) are 2.2 per 100,000. Over 111,000 people in the U.S. suffered MRSA infections in 2005, coming to 38 people per 100,000 population, with 18,650 deaths, per the CDC, According to the MRSA Survivors Network, other organizations estimate these MRSA numbers to have been far higher.
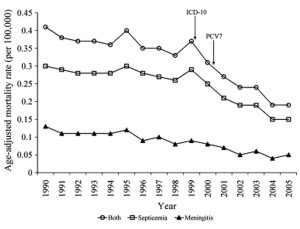
Graph from Pulido M, & Sorvillo F., suggests an increased speed of reduction in pnumococcal deaths since the vaccine began in year 2000.
UCLA researchers suggested that a few hundred U.S. deaths per year are being saved
by the pneumococcal vaccine introduction. By contrast, a USA Today investigation finds the number of yearly U.S. MRSA deaths to be close to 23,000 deaths per year.
That’s two and a half times all the ebola deaths in Africa as of Feb 2015. Here. Every year.The number of yearly U.S. MRSA deaths per citizen is more than triple the rate of U.S. polio deaths during the peak of the polio epidemic (polio deaths reached 3,000 in 1952, with half of today’s population).
Please “Like” Baby Poop
No Drop in Hospitalizations After Vaccine Introduced
As a result of vaccinations, meningitis deaths dropped 70% from 1980 to 2007, from 4.7 to 1.4 cases per 100,000. According to the CDC, the rates for all U.S. pneumonia hospitalizations in children under 2 years have dropped by about one third since the introduction of pneumococcal vaccines—but not for children aged 2 to 4—and the overall rate of all-cause (non-birth-related) hospitalizations has not dropped in infants or in young children.
More on MRSA in Children
Now far from being a chiefly hospital-acquired infections, a 2013, NIH-supported study reported that 60 to 70% of MRSA infections in children are being acquired in the community. Swedish researchers have found S. aureus to be living in infant intestines at an increasing rate over recent decades and are now finding it in 73% of infant stools. Although no particular problem with intestinal staph illnesses has been recognized, from this gut home, staph can provide a reservoir to seed infections in other body areas when immune defenses are down.
Is the Epidemic Slowing?
Some sources are claiming gradual drops in hospital-acquired infections since 2005 but community infections remain strong. A large 2013 analysis suggests continued MRSA growth. Of great concern, several medical studies report that rates have continued to climb in intensive care units for tiny newborns and for hospitalized children.
Key Points:
> In our human microbiome, certain opportunistic bacteria are maintained so that they keep out much more serious microbes.
> It’s becoming evident to researchers that pneumococci and S. aureus have been competitors within human microbiomes.
> Staph aureus has replaced part of the niche in our microbiota created by the reduction of pneumococcal bacteria via pneumococcal vaccines.
> Over-use of antibiotic drugs created MRSA and the reduction of pneumococcal bacteria from the human microbiome has allowed MRSA to flourish.
> The increase in S. aureus is responsible for 60 times as many deaths as the pneumococcal vaccine has saved.
> MRSA is no longer something to catch only from medical procedures, it has become widespread throughout the community.
> MRSA deaths were reported at 6.5 in 100,000 population in 2005.
References:
Acton, D. S., et al. Intestinal carriage of Staphylococcus aureus: How does its frequency compare with that of nasal carriage and what is its clinical impact? Eur J Clin Microbiol Infect Dis 278, no. 2 (Feb 2009):115–27. “In young children the colonization of the intestines with S. aureus occurs at a very high frequency within the first 6 months of life”
Blaser, M. J., & Falkow, S. What are the consequences of the disappearing human microbiota? Nat Rev Microbiol 9, no. 12 (Dec 2009): 887–94. “A growing body of evidence indicates that the encapsulated pneumococci and S. aureus are ecological competitors93, 94, and that the loss of the former is leading to the expansion of the latter95.”
Bogaert, D., et al. Colonisation by Streptococcus pneumoniae and Staphylococcus aureus in healthy children. Lancet 263, no. 9424 (Jun 2004): 1871–2. “These findings suggest a natural competition between colonisation with vaccine-type pneumococci and S aureus, which might explain the increase in S aureus-related otitis media after vaccination.”
Carey, AJ & Long, SS. Staphylococcus aureus: a continuously evolving and formidable pathogen in the neonatal intensive care unit. Clin Perinatol 37, no. 3 (Sep 2010): 535-46. “a global epidemic because of virulent community-associated MRSA (CA-MRSA)… has moved into neonatal intensive care units (NICUs).”
Centers for Disease Control and Prevention (CDC). Pneumonia hospitalizations among young children before and after introduction of pneumococcal conjugate vaccine–United States, 1997-2006. MMWR Morb Mortal Wkly Rep 58, no. 1 (Jan 2009): 1–4. “The rate for all-cause pneumonia among children aged 2–4 years did not change after PCV7 licensure and has remained stable.”
Chowdhary, S. & Puliyel, J. Incidence of pneumonia is not reduced by pneumococcal conjugate vaccine. Bull World Health Organ 86, no. 10 (Oct 2008): A. “Beutels6 has cautioned against this trend of noting the “positive” uncertainties (herd immunity, protection beyond 2.5 years) without reporting the “negative” ones (serotype replacement,7 increased incidence of asthma),8 which could dampen enthusiasm for the intervention.”
Daily Briefing, Hospital MRSA cases drop by 54%. The Advisory Board (Sept 18, 2013). “The number of serious MRSA infections diagnosed in people at home decrease by 5%.”
David, M. Z., & Daum, R. S. Community-associated methicillin-resistant Staphylococcus aureus: Epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev 23, no. 3 (Jul 2010): 616–87. “Since the mid-1990s, however, there has been an explosion in the number of MRSA infections reported in populations lacking risk factors for exposure to the health care system.”
Dolapo, O., et al. Trends of Staphylococcus aureus bloodstream infections in a neonatal intensive care unit from 2000-2009. BMC Pediatr 14 (May 2014): 121. “Increased severity of staphylococcal infections and associated rising mortality are possibly related to the increasing MRSA infections with a more virulent community-associated strain.”
Dukic, V., et al. Epidemics of Community-Associated Methicillin-Resistant Staphylococcus aureus in the United States: A Meta-Analysis. PLOS one 8, no. 1 (Jan 2, 2013). “Our analysis reveals a dramatic increase in infections over the past two decades, with CA-MRSA strains now endemic at unprecedented levels”
Eisler, P., Dangerous MRSA Bacteria Expands Into the Communities. USA Today (Dec 16, 2013). “according to hospital billing data collected by the U.S. Agency for Healthcare Research and Quality. The data suggest those hospitalizations resulted in nearly 23,000 deaths.”
Evans, R. The silent epidemic: CA-MRSA and HA-MRSA. Amer Acad Ortho Sur 7, no. 12 (May 2008). Accessed Dec 13, 2012. “The number of hospital admissions for MRSA has exploded in the past decade. By 2005, admissions were triple the number in 2000 and 10-fold higher than in 1995.”
FDA Contributing to Fight Against Polio. FDA Consumer Health Information. U.S. Food & Drug Administration (April 2013). “At the height of the epidemic in 1952, there were more than 3,000 [U.S.] deaths.” Google: The U.S. population was 157,600,000 in 1952; just over half that in 2005.
Hannah, B., MRSA Statistics 2005 Data. “Other organizations estimate the true numbers to be over one million infected in the US with MRSA and over 100,000 deaths.”
Hayward, A., et al. Increasing hospitalizations and general practice prescriptions for community-onset staphylococcal disease, England. Emerg Infect Dis 14, no. 5 (May 2008): 720–6. “Hospital admission rates for staphyloccocal septicemia, staphylococcal pneumonia, staphylococcal scalded-skin syndrome, and impetigo increased >5-fold.”
Iwamoto M., et al. Trends in invasive methicillin-resistant Staphylococcus aureus infections. Pediatrics 132, no. 4 (Oct 2013): e817-24. “there were no significant reductions in health care-associated MRSA infections in children. Concurrently, the incidence of [community acquired] MRSA infections has increased”
Klein, E., et al. Hospitalizations and deaths caused by methicillin-resistant Staphylococcus aureus, United States, 1999-2005. Emerg Infect Dis 13, no. 12 (Dec 2007): 1840–6.
Klevens, R. M., et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA 298, no. 15 (Oct 2007): 1763–71. “In 2005, the standardized mortality rate was 6.3 per 100,000.”
Lindberg, E., et al. Long-time persistence of superantigen-producing Staphylococcus aureus strains in the intestinal microflora of healthy infants. Pediatr Res 48, no. 6 (Dec 2000): 741–7. “infants had S. aureus in their intestines, which increased to 73% by 2-6 months”
Lysenko, E. S., et al. The role of innate immune responses in the outcome of interspecies competition for colonization of mucosal surfaces. PLoS Pathog 1, no. 1 (Sep 2005): e1. “This study demonstrates how innate immune responses may mediate competitive interactions between species and dictate the composition of the colonizing flora.”
Morita, J. Y., et al. Association between antimicrobial resistance among pneumococcal isolates and burden of invasive pneumococcal disease in the community. Clin Infect Dis 35, no. 4 (Aug 2002): 420–7. “The increasing prevalence of multidrug-resistantpneumococci among children may be leading to an increase in invasive disease.”
Park, B., et al. Role of Staphylococcus aureus catalase in niche competition against Streptococcus pneumoniae. J Bacteriol 190, no. 7 (Apr 2008): 2275–8. “Recent reports of increased S.aureus colonization among children receiving pneumococcal vaccine implicate Streptococcus pneumoniae as an important competitor for the same niche.”
Pulido M. & Sorvillo F. Declining invasive pneumococcal disease mortality in the United States, 1990-2005. Vaccine 28, no.4 (Jan 22, 2009): 889-92. (Figure 1 shows increase in rate of decline after introduction of vaccine.)
Rana, D., et al. Staphylococcus aureus, including community-acquired methicillin-resistant S. aureus, in a level III NICU: 2001 to 2008. Am J Perinatol 29, no. 6 (Jun 2012): 401-8. “The incidence of MRSA (colonization and infection) nearly doubled during the study period“
Regev-Yochay, G., et al. Association between carriage of Streptococcus pneumoniae and Staphylococcus aureus in Children. JAMA 292, no. 6 (Aug 2004): 716–20. “Streptococcus pneumoniae carriage, specifically of vaccine-type strains, is negatively associated with S aureuscarriage in children.”
Romano, P., Hospitalizations due to skin and soft-tissue infections among children have doubled in the past 10 years. UC Davis Health System (Aug 16, 2011), “children hospitalized… infections, most due to (MRSA), has more than doubled since 2000″


[…] in the U.S. per year, MRSA is clearly of far greater concern than any viral exposure. There’s an interesting link between this infection and vaccines. It turns out that the pneumococcal vaccination program is […]