by Linda Folden Palmer, DC
Reprinted from Dynamic Chiropractic, Jan 1, 2002; Volume 20 (1)
Bone Density: The Big Dairy Fallacy
While the National Osteoporosis Foundation tells us we need more calcium to build stronger bones, especially from cow’s milk, the scientific evidence does not support this.
The Chinese University of Hong Kong performed successive studies in the 1990s analyzing milk and calcium intake as they relate to the growth of children. This was an ideal place and time for such an investigation, because cow’s milk was just making its way into popular use in that country, and the traditional diet was not high in calcium.
The first study looked at children from birth to five years of age. With 90 percent of the study children drinking milk, their average calcium intake was 550 mg. At age five, the current level of calcium intake for each child did not correlate with their bone mineral levels. The calcium intake during the second year of life proved to be the strongest predictor of bone “hardness” at age five (breast milk would provide the same or more advantage as cow’s milk or other sources).1
In the second study, seven-year-old children were given calcium supplements to bring their daily calcium intakes up to 800 mg. Over 18 months no increases were seen in height or arm or leg bone density beyond those not supplemented, although some improvement in spinal bone density was seen.2 At ages 12 to 13, calcium intake did not correlate to bone mineral content, except that the girls who consumed the higher levels of calcium had lower bone density in their arms.3
In all these studies, higher weight and greater physical activity were strongly associated with higher bone mineral content. By adolescence, neither calcium intake nor physical activity had any more influence on bone mineral improvement.4 A 14-year British study found that in young adults, their early teenage body weight and physical activity levels determined their bone mineral densities, with a slight effect from calcium intake.5
In a widely quoted study by a British hospital, researchers provided an extra glass of cow’s milk to adolescent girls’ diets, comparing their growth to those who drank an average of just over one half cup per day. Total daily calcium intake at the beginning of the study was 750 mg, and the extra milk group increased to 1,100 mg. The researchers reported about 10 percent greater bone growth rate for those with the extra milk.6 These children also gained a little more weight, but not height. The reported extra bone density could not be validated by any changes in the blood enzyme markers that typically reflect bone growth and bone re-absorption. Insulin-like growth factor was also found to be higher in the extra milk group.
Several experts wrote replies to this study, which had been paid for by the U.K. dairy industry. One expert, doing his own math from the study, found the milk group to have a slightly lower average total bone mineral content at the end of the study.7
A U.S. study on child twins found some increases in bone density in the arms and spine with calcium supplements (not milk).8 Once puberty began, however, calcium provided no benefits.
While dairy promotions also include praise for the protein of milk as well, this protein may be more of a problem in osteoporosis than calcium could be a solution. The animal proteins of meat and dairy products cause calcium loss.9The level of calcium needed in the diet depends greatly on the animal protein intake.10 For many of the high animal protein diets of Americans, it may not be possible to consume enough calcium in the diet to compensate for the amount lost to these high-acid proteins.11 For this reason, Americans have among the highest osteoporosis rates in the world, while their dairy intake is also among the highest. Doubled animal protein causes 50 percent more calcium loss. Yet, when a high protein intake is soy-based, a positive calcium balance can be maintained with only 450 mg of calcium per day.12
The chief concern over bone density is that it gradually reduces with maturity. At a certain point of bone loss, the term osteoporosis is used. This is a level where low-trauma bone fractures become more frequent. Spinal fractures are a problem, as are hip and arm fractures, which are easier to measure for research purposes. The highest level of bone density attained in young adulthood correlates with bone density maintained in later decades. What is not entirely understood is how much impact dietary factors have on these events. Some studies suggest that childhood calcium intake before puberty may have some slight positive effect. At the same time that diabetes, cancer, and other concerns may limit the amount of dairy that should be given to a child, it also appears that bone protection is no reason to promote dairy consumption beyond childhood.
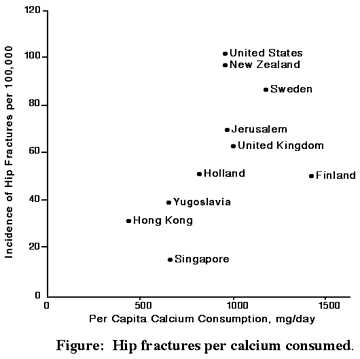
In 1986 a Harvard researcher produced a graph that demonstrated a nearly direct relationship between calcium intake and hip fractures – the more calcium, the more fractures.13,14
A 1987 study of 106 adult women suggested that calcium intake between 500 and 1,400 mg per day led to no difference in bone mineral densities.15
A larger Italian study found that in women who consumed between 440 and 1,025 mg of calcium per day, a slightly increased number of hip fractures occurred with higher milk intakes.16
A recent study of 78,000 nurses found that women who drank more than one glass of milk per day had a 45-percent greater chance of hip fracturescompared to those who drank far less.17 Those who took in the same amount of calcium from nondairy sources saw no such increase, nor a decrease in fractures. Since many studies are performed on women only – they do suffer more osteoporosis – Harvard researchers decided to look at men. They found that those who drank three or more glasses of milk per day, compared to one or less per week, had very slightly fewer hip fractures, but these were balanced by slightly more arm fractures.18 The highest calcium intakes from food and supplements together produced an increase in fractures overall.
The rate of hip fractures in the U.S. for people of many races and ethnic origins is exactly inverse to their rates of lactose intolerance. In other words, those who are likely avoiding milk as adults have the fewest fractures. Non-Hispanic white women have 139 fractures per 100,000 people; Mexican-Americans have 67 per 100,000; and African-Americans average 55 per 100,000.19 The indigenous peoples of South Africa have not traditionally been dairy consumers. Their consumption is still very low, although formula is making great inroads. Those of osteoporosis age today however would not have been raised on formula. Typically, South Africans consume only 200 mg of calcium per day, but their rate of fractures is extremely low – fewer than seven per 100,000 people per year.20 Compare this to their dairy-exposed American counterparts. The milk-drinking (and higher calcium intake) populations around the world are the ones who have osteoporosis as a major problem.21 These rates are increasing in typically low fracture areas around the world as these regions adopt Western practices.
In Japan, as in many other non-Caucasian populations, dairy intake has traditionally been minimal and calcium intakes have been low – and hip fracture rates are low, but have been growing recently,22 as is the portion of adults who were raised on dairy. While industrialization also brings reduced physical exercise, there is a much more consistent common denominator seen in the timing and geographic regions of these bone problems – cow’s milk. While we feel our nutrition is superior today over centuries past, archeological research has shown that Caucasian post-menopausal bone loss in the 18th and 19th centuries was less than that seen today.23 Clearly, high calcium intake, and certainly high dairy intake, are not the prevention for osteoporosis.
Milky Messages
Why the conflicts between the bulk of research findings and the recommendations of the National Osteoporosis Foundation (NOF)? Other funding comes from small and large private donations, with some from the federal government.24 Another big supporter of the NOF is Bozell Worldwide, the marketing firm that created the huge milk mustache campaign for the dairy industry. Only two percent of the NOF’s funding has gone to osteoporosis research.
Good, Bad, and Curious Solutions
Other common foods that are excellent sources of calcium, listed in order of highest amount per calorie, are: molasses; dark salad greens; cabbage; broccoli; green beans; cucumber; peas; soybeans; squash; most types of beans (including cocoa); kiwi; real maple syrup; brown sugar; and tomatoes. In addition to this list is of course human milk. Calcium may also be added to corn tortillas and some orange juice, apple juice, and rice and soy milks. When these foods are the major source of calcium, and meat intake is not high, USRDA levels may be in excess of needs.
The World Health Organization suggests that 400 to 500 mg of calcium per day is appropriate for adults. The United States RDA for calcium is 800 mg for most people one year of age and over and 1,200 mg for teens and pregnant and lactating mothers. Ours is the highest recommendation in the world. Beyond these earlier set standards, the U.S. National Institutes of Health (NIH) has gradually raised its recommendations for calcium requirements: for children six to 10 years old, 800 to 1,200 mg; 11 to 24 years, pregnant, or nursing, 1,200 to 1,500 mg; and over 65, 1,500 mg. They base their decisions chiefly on our increasing osteoporosis problems.
“The preferred source of calcium is through calcium-rich foods, such as dairy products,” asserted the consensus statement of the NIH’s Development Conference on Optimal Calcium Intake.25 It reinforced vitamin D intake too, which is added to milk, and naturally derived from sun exposure or eating fish. It does not, however, mention any of the other nutritional factors that are important for bone development – those that are inadequate in milk. At the same time, the report makes taking calcium supplements sound very complicated.Boron, copper, magnesium, manganese, zinc, vitamin C, and proper fluoride levels are just as important as calcium for optimal bone growth. None of these are high in cow’s milk, so none of these are advertised as important for bones.
Phosphorous is important for bone development as well, but cow’s milk has too much of this, causing decreased calcium availability. This is apparently why phosphorous is not mentioned, either. Nor does NIH mention that reduced animal protein consumption would help calcium levels. (Remember that the beef industry is the other end of the dairy industry.) Deep in the text they mention some other foods naturally high in calcium, but only in reference to vegans, who do not drink milk. This list is rather inaccurate and exclusive, sounding a bit distasteful (collard greens and sardine bones). They also emphasize that a little pain and gas should not prevent the lactose intolerant from having at least two servings of milk per day.
As more problems become apparent with milk, and people buy less, greater measures are taken to encourage milk-drinking. The new motto for the government’s Healthy People 2000 initiative is, “at least three cups of milk every day” for “every body.” The NIH, whose initial intentions are often better than its final reported conclusions, funded half of the huge 1997 study that showed that nurses have more fractures when consuming more milk. To date, however, it has not changed its recommendations about milk consumption.
All the while, the American Dietetic Association, with grants from the dairy industry, continues to publish reports such as “Many Asian American elderly consume an inadequate amount of dietary calcium.”26 Their conclusions were based on milk consumption, not their bones. It’s obvious what their recommended solution was. A recent dairy commercial shows young men playing basketball outside (i.e., exercising and soaking up vitamin D), which are two great ways to build stronger bones. A milk carton stands alongside urging them to go inside, sit down, and have some milk for their bones.
Dutch dairy researchers have come up with a new milk product designed to be better for bone health. They increased the calcium content and lowered the protein, phosphorus, and fat content – in other words, they lowered the dairy content. Not surprisingly, elderly people taking this new low-milk calcium supplement lost less calcium each day than those drinking normal milk.27
Deflating Dairy
The norms promoted as desirable for childhood growth rates and puberty are based on a comparison of those who consume bovine growth hormones (natural in all milk, and often additionally supplemented), early and regularly, to those who are raised on natural foods. While the same height is achieved in the end, with obesity more common on the side of dairy consumers,28 those with the so-called superior nutrition experience a traumatic increase in cancer, heart disease, diabetes, and many other diseases.
The highly promoted idea that milk builds “strong bones” refers to the prevention of osteoporosis – this is the reason for strengthening bones. Decades of effort to demonstrate that high calcium diets chiefly derived from dairy products build strong bones have failed to prove any such correlation. In fact, the opposite seems to be true.29 It appears that high calcium intake before puberty, and especially in young childhood, may have some slight positive effect on bones, but this diet is not the answer. A balanced intake of all the bone minerals, along with adequate vitamin A, C, and D, is what is truly needed. A balanced intake of minerals cannot occur when the diet emphasizes dairy. Dairy’s high calcium content causes relative deficiencies in magnesium and other bone-building minerals, and its high phosphorus and animal protein reduces calcium availability. Physical activity has the greatest benefit – the body efficiently uses what is available to build strong bones when it senses the need. Human milk and vegetable sources are superior to dairy for calcium and other nutrients in many ways. There are fewer nutritional or other health advantages to giving cow’s milk to children than is generally believed, while there are certainly many risks.
If you pay attention to health research announcements in the news, you will notice that almost every day another finding is made about whole grains; soy; a serving of vegetables; two fruits per day; cashews; legumes; fish; or some other food – other than milk, that is – and their connection to a reduced risk of heart disease, breast cancer, stroke, diabetes, or other diseases. This is because cow’s milk and its derivatives today make up one third of the adult diet and half to two-thirds of caloric intake in children, thus replacing so much other important, nutritious food needed in the diet. This leads to insufficient intake of some important vitamins, several minerals, and healthy fiber and vegetable oils.Cancer-preventing antioxidants in foods are missing in the milk diet. While one form of anti-oxidant vitamin A is added to milk (but not all dairy products), and likely counteracted by the pesticide and drug residues, the full complement of vitamin A and associated enzymes found in vegetables and other foods are required for cancer prevention. Many more kinds of antioxidants are found in vegetables, legumes, fruits, and grains.
References
- Lee WT, et al. Relationship between long-term calcium intake and bone mineral content of children aged from birth to 5 years. Br J Nutr (Hong Kong) 1993;70(1):235-48.
- Lee WT, et al. A randomized double-blind controlled calcium supplementation trial, and bone and height acquisition in children. Br J Nutr (Hong Kong) 1995;74(1):125-39.
- Cheng JC, et al. Determinants of axial and peripheral bone mass in Chinese adolescents.Arch Dis Child (Hong Kong) 1998;78(6):524-30.
- Cheng JC, et al. Axial and peripheral bone mineral acquisition: a 3-year longitudinal study in Chinese adolescents. Eur J Pediatr (Hong Kong) 1999;158(6):506-12.
- Fehily AM, et al. Factors affecting bone density in young adults. Am J Clin Nutr (England) 1992;56(3):579-86.
- Cadogan J, et al. Milk intake and bone mineral acquisition in adolescent girls: randomised, controlled intervention trial. BMJ (England) 1997;315(7118):1255-60.
- Griffiths ID, Francis RM. Results in two groups are not so different. BMJ (England) 1998; 316(7146):1747-8.
- Johnston CC, et al. Calcium supplementation and increases in bone mineral density in children. N Engl J Med 1992;327(2):82-7.
- Breslau NA, et al. Relationship of animal protein-rich diet to kidney stone formation and calcium metabolism. J Clin Endocrinol Metab 1988; 66(1):140-6.
- Barzel US, Massey LK. Excess dietary protein can adversely affect bone. J Nutr 1998; 128(6):1051-3.
- Allen LH, et al. Protein-induced hypercalcuria: a long-term study. Am J Clin Nutr 1979;(4): 32741-9.
- Zemel MB. Calcium utilization: effect of varying level and source of dietary protein. Am J Clin Nutr 1988; suppl.48(3):880-3.
- Hegsted DM. Calcium and osteoporosis. Adv Nutr Res 1994;(9);119-28.
- Hegsted DM. Calcium and osteoporosis. J Nutr 1986;116(11);2316-9.
- Riggs BL, et al. Dietary calcium intake and rates of bone loss in women. J Clin Invest1987;80(4):979-82.
- Tavani A, et al. Calcium, dairy products, and the risk of hip fracture in women in northern Italy. Epidemiology (Italy) 1995; 6(5);554-7.
- Feskanich D. et al. Milk, dietary calcium, and bone fractures in women: a 12-year prospective study. Am J Public Health 1997;87(6);992-7.
- Owusu W, et al. Calcium intake and the incidence of forearm and hip fractures among men.J Nutr 1997;127(9):1782-7.
- Bauer RL. Ethnic differences in hip fracture: a reduced incidence in Mexican Americans.Am J Epidemiol 1988;127(1):145-9.
- Abelow BJ, et al. Cross-cultural association between dietary animal protein and hip fracture: a hypothesis. Calcif Tissue Int 1992;50(1):14-8.
- Cooper C, et al. Hip fractures in the elderly: a world-wide projection. Osteoporosis Int1992;2(6):285-9.
- Fujita T. Osteoporosis in Japan: factors contributing to the low incidence of hip fracture.Adv Nutr Res (Japan) 1994;989-99.
- MacLennan WJ. History of arthritis and bone rarefaction evidence from paleopathology onwards. Scott Med J (England) 1999;44(1):18-20.
- Cohen R. Who is behind the National Osteoporosis Foundation and what is their agenda? Dairy Education Board Archives, www.notmilk.com, May 23, 1999: 1-5.
- Optimal calcium intake. NIH Consens Statement 1994;(4):121-31.
- Kim KK, et al. Nutritional status of Chinese, Korean, and Japanese-American elderly. J Am Diet Asso. 1993;93(12):1416-22.
- van Beresteijn EC, et al. Relationship between the calcium-to-protein ratio in milk and the urinary calcium excretion in healthy adults – a controlled crossover study. Am J Clin Nutr(Netherlands) 1990;52(1):142-6.
- Rolland-Cachera MF, et al. Influence of macronutrients on adiposity development: a follow up study of nutrition and growth from 10 months to 8 years of age. Int J Obes Relat Metab Disord (France) 1995;19(8):573-8.
- Kushi LH, et al. Health implications of Mediterranean diets in light of contemporary knowledge. 1. Plant foods and dairy products. Am J Clin Nutr 1995;61(suppl 6): 11407S-1415S.
Linda Folden Palmer, DC
San Diego, California
![]()

No Comments